By now, the numbers are familiar: a woman dies of cervical cancer every 90 seconds. There are more than 600,000 cervical cancer cases globally per year, and some 350,000 deaths. That’s more than 1.5 million women dying every five years from a disease that, for the past 17 years, has been mostly preventable.
Less familiar is the fact that cervical cancer cases are on the rise, projected to go up almost 50% over the next 17 years. Protection from the HPV vaccine that prevents human papillomavirus infections, which give rise to most cases of cervical cancer, stands at only 1 in 8 girls worldwide. Acceptance is low and the costs are high: it strikes women in their prime family and career-building years and leaves an estimated 210,000 orphans every year.
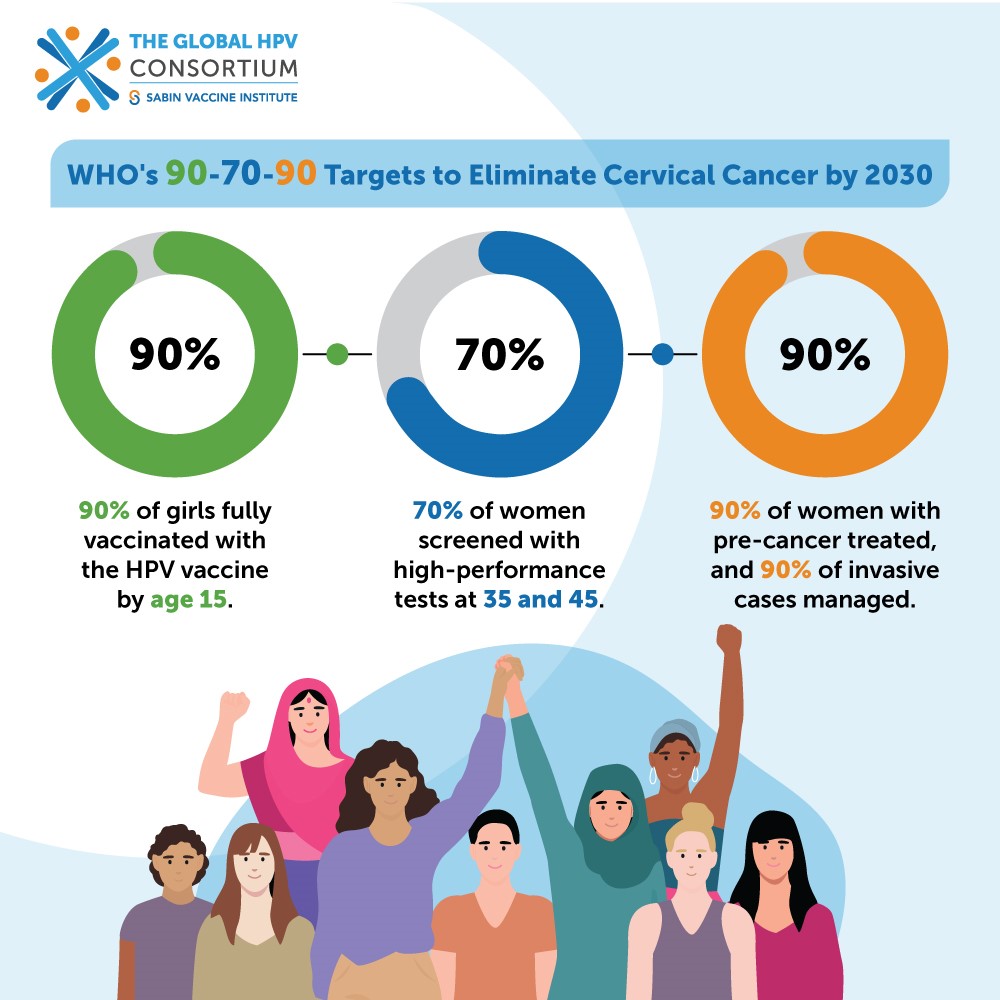
The worsening situation raised clarion calls to end cervical cancer, with the tantalizing goal of targeting the first cancer ever for elimination. In 2018, the World Health Organization announced a global call for action to eliminate cervical cancer. In 2020, the World Health Association adopted a global strategy including 90-70-90 targets (percentages of women vaccinated, screened and treated) by 2030.
To answer the calls and create a plan that might reach these ambitious targets, the Global HPV Consortium, led by the Sabin Vaccine Institute, is launching in Kuala Lumpur this week. The aim: actionable steps to quicken the pace of HPV prevention and cervical cancer elimination.
It’s clear this Consortium cannot be business as usual with a traditional immunization playbook. We start by bundling HPV vaccination, screening, and treatment together. None of these approaches can singly achieve cervical cancer elimination – vaccination remains primary prevention, but secondary prevention (screening and treatment of precancerous lesions) is vital for vigilance and early cure. Equally important is for immunization, non-communicable diseases, cancer-control and HIV programs to coalesce.
We are committing to creating new alliances and partnerships, building a novel trans-disciplinary ecosystem that strategically connects all those who can effect change – from health workers in the field to adolescents, youth and women, community influencers, advocacy groups for vulnerable populations such as women with HIV, gender-focused organizations, professional bodies, industry, supply chain providers and non-profits.
Using lessons learned from the pandemic, we know the current environment requires political will and sustainable financing as well as community-based partnerships, advocates, and training and communication to move the needle on vaccine demand.

Many times, during my career in public health, fresh thinking drove outcomes. Sometimes the solution was rooted in communities, as when we leveraged a million local ASHAs (Accredited Social Health Activists) for doorstep delivery of free contraceptives and pregnancy testing kits throughout India and for promoting in-hospital births, dramatically reducing maternal mortality. Sometimes it was new ways of framing data, such as quantifying, locating and vaccinating consistently missed children, to finish polio in India.
The challenges facing HPV prevention and cervical cancer elimination require innovation and creativity. After almost two decades, many still don’t make the connection between HPV and cervical cancer, and many are waylaid by misinformation. It’s time for new language, new approaches, new collaborations…and a new Consortium to bring the many exciting possibilities to life.
More information on the Global HPV Consortium here: https://www.sabin.org/the-global-hpv-consortium/




