In the autumn of 1918, a global influenza outbreak began that would claim more lives than World War I (or the Great War). The war itself, which ended in November 1918, had a significant impact on how the virus spread around the world – and even influenced the name Spanish Flu.
There was nothing particular ‘Spanish’ about the flu: it didn’t begin in Spain and, while the country was badly affected, it wasn’t hit any harder than others. (The first wave spread in US military camps in 1917.)
However, Spain remained neutral during the conflict and its papers freely reported the outbreak. Media in France, the United Kingdom, Germany, the United States and elsewhere played down the impact on their own country in a bid to keep up morale. Newspapers were either directly controlled by national governments or keen to self-censor in the interest of patriotism at a time of war. They all happily reported on events in Spain – leading many to incorrectly presume that the Iberian Peninsula was the epicentre.
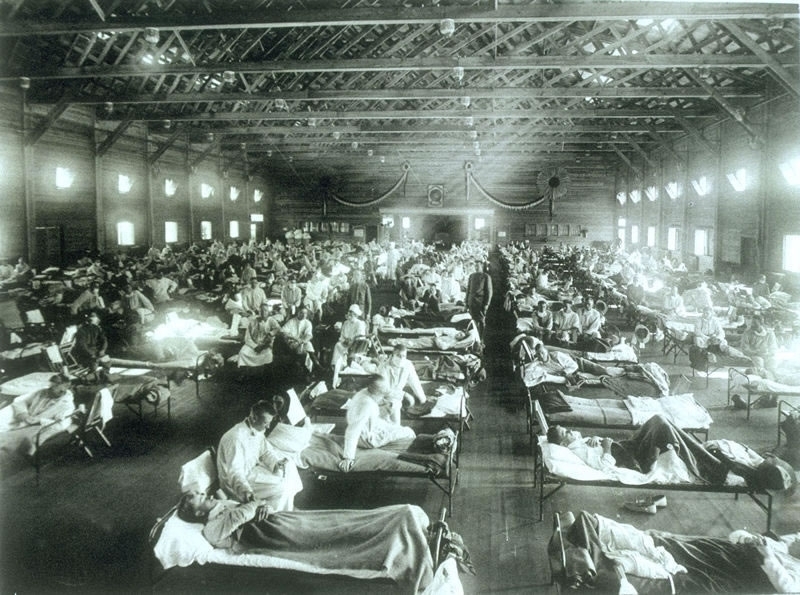
In summer of 1918, the virus spread among military units who lived in cramped quarters. And, as the war ended, surviving solders returned home – bringing influenza with them.
After four gruelling years of conflict, the immediate post-war period was a time for celebration. Public gatherings present an ideal opportunity for infectious diseases to find new victims. This most likely prolonged the second wave of the outbreak.
A third wave in the early spring of 1919 took war-weary populations by surprise, claiming millions more lives. Just as with seasonal influenza, the worst-hit populations were the very old and the very young. However, in comparison to a typical flu epidemic, there was a major spike in the 25-34 age group. Many soldiers who survived the trenches, did not survive the flu. Some returning soldiers shared the lethal virus with their spouses, also helping to push up the fatality rate in young adults.
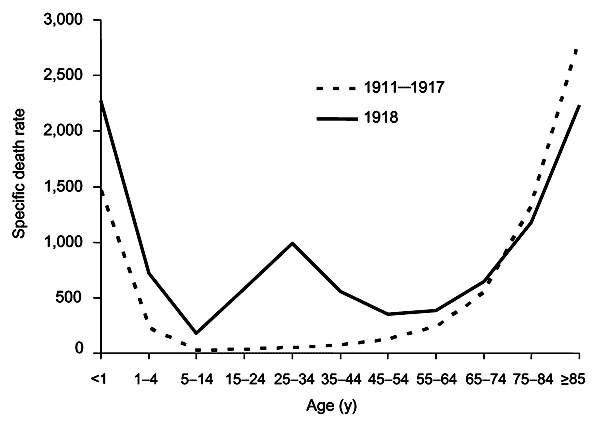
There are a number of other reasons why the proportion of deaths among young adults was higher than normal. For one thing, the older population had partial immunity from the 1889-1890 flu pandemic (known as Russian flu).
The virus has also been shown to have triggered what is known as a ‘cytokine storm’ – an immune response that can be particularly severe in those with stronger immune systems.
The worst-affected group of all were pregnant women. Of the pregnant women who survived, over one quarter is estimated to have lost the child.
(Pregnant women are the #1 priority for flu vaccination, according to the WHO.)
During the 1918-1919 pandemic, researchers tried to develop a vaccine. According to the History of Vaccines project, a number of vaccines were tested against Bacillus influenzae (now known as Haemophilus influenzae) as well as strains of pneumococcus, streptococcus, staphylococcus, and Moraxella catarrhalis bacteria. These bacterial vaccines had no chance of stopping the pandemic which, we now know, was caused by a new strain of the influenza A virus.
Where are we now?
In the 100 years since the Spanish flu outbreak, there have been four influenza pandemics: 1957-1958, 1968-1969, 1977-1978, and 2009-2010. None were as lethal as the 1918 outbreak.
However, annual outbreaks of seasonal influenza cause between 290,000 and 650,000 deaths per year globally. The death rates are lower because (a) vaccines are available (b) healthcare and hygiene is vastly superior than conditions a century ago and (c) the viruses that cause seasonal flu are less dangerous – and less likely to be fatal to those infected.
Nonetheless, flu viruses can change from one year to the next. Experts continue to worry that a new flu virus could some day emerge with the potential to cause the kind of destruction seen in 1918.
The WHO is warning that low uptake of seasonal flu vaccines in Europe, is leaving vulnerable people at risk should an outbreak occur. Fewer than one third of older people are vaccinated in half of the 53 countries making up the WHO’s European region.
In fact, vaccination rates among high-risk groups have fallen in the years since the 2009-2010 pandemic.
‘Vaccination is the most effective measure to prevent severe disease caused by influenza. However, according to our research, influenza vaccination uptake has been steadily declining in a number of countries in the European Region,’ says Dr Zsuzsanna Jakab, WHO Regional Director for Europe. ‘This is of serious concern now for people at higher risk of severe consequences, especially older people, and in the future potentially for the entire population, as the production of pandemic vaccines is closely linked to seasonal vaccine use.’
In the EU, health ministers have set a target of vaccinating 75% of citizens in high-risk groups. With the exception of the UK and the Netherlands who have met this goal and are consistently above or close to the target, most EU countries are a long way from reaching their goal.
‘All European Union Member States have signed up to the goal of reaching 75% uptake among older people and other vulnerable groups; however, these targets are not being reached,’ says Dr Andrea Ammon, Director of European Centre for Disease Prevention and Control (ECDC).
As we prepare to mark the centenary of the worst flu pandemic in recorded history, it is time to step up efforts to improve flu vaccine uptake.
Older people at higher risk of death from influenza
The WHO estimates that over 44,000 people die annually of respiratory diseases associated with seasonal influenza in the WHO European Region, out of a total of up to 650,000 global deaths.
According to annual surveys for the ECDC and WHO, although 34,000 (over 75%) of these deaths in Europe are among people aged 65 years or above, vaccine uptake remains low in this group. Half the countries in the WHO European Region are vaccinating fewer than one in three older people.
As for the other at-risk groups:
- vaccination was generally recommended for people with chronic illnesses; however, coverage was below 40% in most countries;
- almost all countries recommended influenza vaccination for health-care workers, but the majority reported influenza vaccine uptake as being as low as 40%;
- in total, 90% of countries had vaccine recommendations for pregnant women in 2014/2015, compared with 40% before the 2009 A(H1N1) pandemic; however, coverage overall was low, with half the countries reporting uptake below 10%;
- fewer than half the countries, most of them in eastern Europe, recommended influenza vaccination for young children; vaccination coverage ranged from less than 1% to 80%.





Prudhvi Reddy
April 27th, 2020
“However, annual outbreaks of seasonal influenza cause between 290,000 and 650,000 deaths per year globally.”
Jon
May 2nd, 2020
According to the numbers of the coronavirus infected patients…we are NOT ready for a pandemic.
Ryan
May 24th, 2020
Haha Haha so funny bahahaha. It’s totally not like the government of every country put in laws to stop it but no one listens so the only reason we aren’t prepared is because of stupid people. Hahahaha
Hhgty
May 25th, 2020
Question asked 2018 and Pandemic in 2020! Isn’t this amazing!
Gary Finnegan
May 25th, 2020
Experts have warned about pandemics for years. Most expected it to be a new strain of flu virus, but a new coronavirus was also possible (see SARS, MERS).
The 2011 film Contagion lays this out in great detail, presumably based on consulting with experts. (I’m not saying it’s a great film!)
LOVELL
June 9th, 2020
Correct – prophetic!
Pingback
May 26th, 2020
[…] * Graph from Vaccines Today, Oct. 24, 2018, https://www.vaccinestoday.eu/stories/100-years-spanish-flu-world-ready-next-pandemic/ […]
Hajar lakrati
May 26th, 2020
I was reading about Spanish flu in order to understand the current Pandemic. I was surprised when I seen the date of this article and most importantly it still feels like 1918 still. I wonder how far did we truly advance medically ! After months we still cannot figure out how this virus operates. People are doing their own research to make sense out of this. All those funds we contributed to medical research I am disappointed to see the results of covid 19 and even more worst not a single study concluded about this virus. Just random theories like 1918 🙂
Gary Finnegan
May 26th, 2020
I wouldn’t agree – a huge amount has been learned about the new coronavirus in a short time. True, there is no cure or vaccine yet.
Bill Els
May 30th, 2020
Social media is being swamped by conspiracy theories. The attack on Bill Gates centres on the supposed implanting of nano chips when we are injected with the vaccine (wen it is developed). The rationale is that Gates has experimented on poor people in Afrika and the implants will turn us into human robots, controlled by the illuminati. Such nonsense, why go to all the trouble of inventing a new virus and antidote vaccine when you are already vaccinating thousands with the common flu vaccine?
Amaka
June 22nd, 2020
Bill Els I hope you’ll be in forefront of those who’ll take the vaccine before its given to others. Ensure that it is the same strain that is given to you, that is given to others.
Pingback
June 23rd, 2020
[…] this, vaccination rates have astonishingly decreased since 2010, particularly among older groups that are more vulnerable to seasonal flu. This decrease in […]
Patrick McMahon
July 6th, 2020
Not knowing much about vaccines,
Could I ask please, Is there any chance that some of the “Spanish flu” vaccine
trials that were discarded, could be retested? With today’s technology could a an old failure be adjusted for c19 ?
Gary Finnegan
July 7th, 2020
Hi Patrick,
there were no ‘Spanish flu’ vaccine trials at the time. The first flu vaccines arrived more than a decade after that pandemic. Also, influenza viruses and coronaviruses are quite different. However, you have a good point about resurrecting previous research. Work on a SARS virus helped give scientists a head-start in searching for vaccines against COVID-19 as the viruses causing these illnesses are quite similar. Some new technologies (such as mRNA vaccines) are being tested against coronavirus. As they are new, it is impossible to say whether they will be proven safe and effective. Time will tell, and we’ll know in the coming months.
Alex Onduko Orumi
July 7th, 2020
God knows.
Michal
December 21st, 2020
It is very crazy how the there is a pandemic every 100 years, Everyone was right about there being a pandemic in 2020 and there was. Please reply for ideas what the next pandemic could be in 2120
Zak
January 2nd, 2021
As u will note in the article there have been several major flu outbreaks last century.
Gana sekhar
April 30th, 2021
spanich 1920vaccine
Angel
August 3rd, 2021
Read about patterns and cycles. It’s nature. Iwhen you become aware about it, you’ll see it in almost everything. From plants, nature, our body, even moods, behaviour, financial markets, economy has patterns and cycle. Also viruses. Seacch golden ratio
renae thomas
August 27th, 2021
I agree! There is a patten around 100 years, yet the flu seems very similar!
A name
December 10th, 2021
COVID-19 hit in november of 2019, not 2020, but it hit more people in 2020 than it did that november
Natalie Lauren Wilkinson
December 27th, 2020
I think the next pandemic will be sooner than 2120…
David
September 12th, 2021
First, the world was ready for the next Pandemic in 2017, but it started going downhill from there. The following article provides the details. But short story is: starting under Bush 1, a National Pandemic response plan was created. Subsequent administrations refined the plan with knowledge gained dealing with new pandemics. The Trump administration even put out their own refined plan in 2017 (linked below). And then not only didn’t follow it, they systematically dismantled every protection in place that might have stopped it early.
https://www.theatlantic.com/politics/archive/2020/06/how-white-house-coronavirus-response-went-wrong/613591/?fbclid=IwAR3n_8uaVs4m_Rrxuxb8QEIMsHGRFqysaAxgybBOMMD62_Azu1bgt26vPKU
https://www.cdc.gov/flu/pandemic-resources/pdf/pan-flu-report-2017v2.pdf
H1N1 (Spanish flu) is still around and infecting/killing people every year. If you get a flu shot, you are getting what experts think is the most likely strain for the coming flu season. The 2009-2010 Swine Flu Pandemic was a novel (new) strain of H1N1. Don’t remember that as being a Pandemic? That’s because the current administration followed the Pandemic Plan. Ebola? Same game plan. Same result. Potential pandemic stopped. How about MERS? Far more deadly form of Coronavirus, although not as transmissible as COVID-19, but it largely went nowhere. And each time they dealt with a new potential pandemic, they got better at dealing with them.
What changed with COVID-19? As the article above mentions, there was no longer any CDC presence in China this time. The last observer left in 2018. And even when the Chinese doctors put out the warning that this was something serious, there was no one around to listen. And this virus behaved differently than all previous viruses, in that it was infectious before the patient was symptomatic (with all previous viruses, you weren’t in danger of spreading the virus before you were very obviously sick). This is one of the reasons for conflicting mask guidelines (the other was the lack of masks for frontline workers, who were at far greater risk than the average person in the first months of the pandemic). The National stockpile for Pandemic Response had been allowed to dwindle beginning in 2017, so there was very little left in 2020. And most PPE in 2020 was made in China, which said it was using all that it was producing.
But one of the biggest differences with the current pandemic compared to previous pandemics is with the American response. In all previous pandemics, the United States would take the lead in the International response. With COVID, the world once again turned to the US for leadership, but it wasn’t there.
Someone asked about the graph. It is a graph of expected deaths versus actual deaths. Statisticians look at previous years and can predict how many people will die in future years (from natural causes, infections, disease, accidents, etc). This graph plots expected deaths per 100,000 people versus age group. Note in 1918, infant mortality was still fairly high. But as the article says, they 25-34 group experienced a very large gain in 1918 (as did most other groups, just not as large). There are similar graphs for expected deaths versus actual deaths for 2020 and 2021 that show that COVID deaths are probably being undercounted, as the expected deaths are far above the number of COVID deaths. And some groups were way down: traffic deaths were down, especially for the middle of 2020. Flu deaths for winter 2020-2021 were a fraction of what they normally are, due to COVID precautions (masks, hand washing, social distancing, small or non-existent seasonal gatherings, school closings, etc). There are some deaths that might not be happening were it not for COVID restricting patients seeking or being able to get medical help (heart attacks, strokes, etc), but not enough to make up the difference between expected and actual deaths (minus COVID).
Nino
September 14th, 2021
Well i guess UK had the most casualties from Covod-19 in Europe, though they had most people Vaccined against flu as you stated that those who got Vaccines against Flu had better chances of surviving , i guess that was not the case.