It is an exciting possibility: the 53-country WHO European Region has the tools and momentum to end the scourge of rubella. Quietly but effectively, more countries than ever have been certified as ‘rubella free’, meaning they have interrupted transmission for three consecutive years.
Region-wide elimination could finally be on the horizon ‒ something which has already been achieved in the Americas. Ensuring high rates of routine immunisation is critical. Uptake of rubella vaccine in the European region stood at 94% in 2021, a slight drop from the 96% recorded in 2019, before the COVID-19 pandemic. Health authorities are working to keep vaccination on track following periods of pandemic-related disruption, with some introducing catch-up programmes for those who missed out.
Through vaccination and close disease monitoring, a solid majority of countries have stopped the spread of a virus that can cause severe heart defects and a range of other developmental issues to the unborn child of a woman if she contracts the disease during pregnancy. For health systems, congenital illnesses are also associated with higher care needs. However, vaccines can protect against this infection, allowing more people to live full and active lives.
Important: The rubella vaccine is usually given in combination with the measles vaccine and is usually administered in childhood and adolescents. It can also be given to adults but unlike flu, pertussis and COVID-19 vaccines, they must not be administered during pregnancy.
In an interview with Vaccines Today, Dr Mark Muscat, technical officer at the WHO Regional Office for Europe, discusses the need to continue the elimination drive by ensuring at least 95% uptake of rubella vaccines (which is combined with measles vaccine).
What is rubella?
Mark Muscat: Rubella is an acute infectious disease caused by the rubella virus. The disease is characterised by a mild, maculopapular rash which occurs in 50%–80% of rubella-infected persons. Adults may experience other symptoms such as low-grade fever and headache. Enlargement of the lymph nodes of the neck, particularly those behind the ear is characteristic and precedes the rash by 5–10 days. Joint pains may occur in up to 70% of adult women with rubella.
Why is it important to eliminate rubella?
Mark Muscat: The public health importance of rubella lies more in its potential to harm the unborn child because the virus can damage the foetus. If a pregnant mother gets infected with the virus in early pregnancy the infection can cause miscarriage, death of the foetus or a constellation of severe birth defects in infants known as congenital rubella syndrome.
Common defects of congenital rubella syndrome include cataracts, congenital heart disease, hearing impairment and developmental delay. Infants with congenital rubella syndrome often present with more than one of these signs but may also present with a single defect, most commonly hearing impairment.
Congenital rubella syndrome (CRS) occurs in up to 90% of live infants born to women infected with rubella during the first 10 weeks of pregnancy. By eliminating rubella virus transmission, we are also preventing congenital rubella syndrome.
How can this be prevented?
The only way we can prevent it is by having a high rubella vaccination coverage in all populations in all countries of the Region. The goal for eliminating rubella is coupled to the goal for eliminating measles since the rubella vaccine is given in combination with the measles vaccine. Achieving and maintaining a high vaccination coverage of at least 95% of the population with two doses will also achieve measles elimination.

What is your current assessment of how the European Region is doing in its attempt to eliminate rubella?
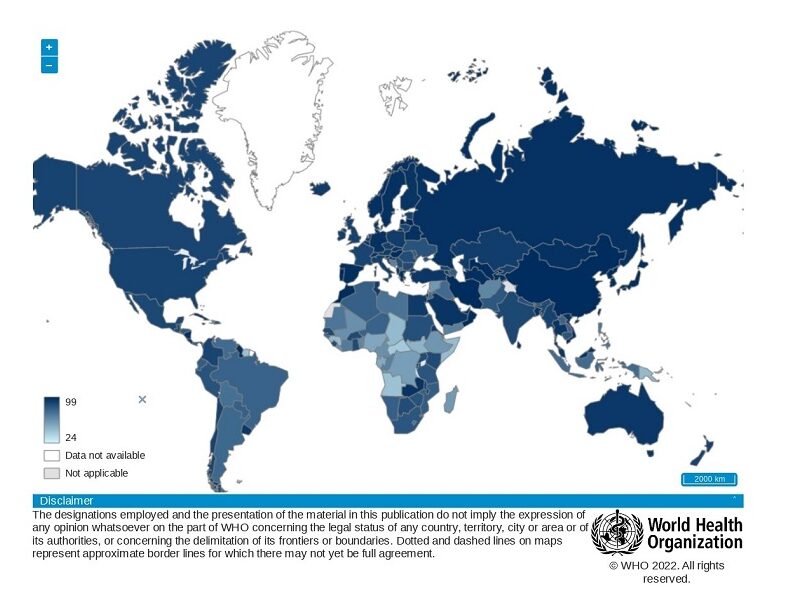
Since 2014, the WHO European Region is progressing well in terms of eliminating rubella as more and more countries are achieving the elimination status. In 2014, 20 countries were considered as having eliminated rubella. By 2019, according to the latest publicly available report of the European Regional Verification Commission for Measles and Rubella Elimination that evaluated the individual country reports, 45 countries were considered to have eliminated rubella. Of these, 29 countries provided evidence for the elimination of both rubella and measles.
The remaining eight countries still need to be evaluated. Five countries had not submitted their report for the 2019 evaluation and three countries are pending a retrospective review including three years of data.
Who needs to do what to accelerate progress on the elimination goal?
To be considered as having eliminated rubella, every country needs to achieve and maintain high rubella vaccination coverage as well as document the absence of ongoing transmission of the disease. This includes information on the quality of rubella surveillance, i.e., the capacity to detect, confirm and monitor the occurrence of the disease.
We do not believe that there is continuously ongoing transmission of rubella in any country in the Region. However, sporadic cases and small and contained outbreaks of rubella may still occur in the Region. Indeed, although very rare nowadays, confirmed congenital rubella syndrome in infants of mothers who were not vaccinated against rubella have been reported.
How did the COVID-19 pandemic affect vaccine uptake and disease surveillance?
The COVID-19 pandemic has adversely affected vaccine uptake and the quality of disease surveillance in many countries in the Region as in the rest of the world.
Utilisation of vaccination services diminished due to restrictions in population movement during full or partial lockdowns to contain the spread of COVID-19. Overall, coverage for measles- and rubella-containing vaccines at Regional level declined by 2% between 2019 and 2020 from 96% to 94%. In 2021, it remained at 94%.
Although one may think that this is a small decline, it does suggest a widening of immunity gaps in some populations. As the number of susceptible individuals grows so does the potential for outbreaks when the rubella virus enters vulnerable communities. Declines in vaccination coverage present a real risk of a resurgence of vaccine-preventable diseases in the Region as COVID-19 public health and social measures are lifted and viruses such as rubella and measles have greater opportunities to spread.
What can be done to address this?
Countries where disruptions in vaccine delivery services have occurred, even for short periods, either at local or national level, are urged to mitigate the accumulation of individuals susceptible to vaccine-preventable diseases. It is therefore of utmost importance that counties put in place an action plan for catch-up immunisations of children who have missed their vaccine doses.
The WHO has published guidance on routine immunisation services during the COVID-19 pandemic and on mitigating the impact of COVID-19 on control of vaccine-preventable disease in the European Region.
Interrupted, or disrupted disease surveillance due to diversion of human and other resources to COVID-19-related matters may have also contributed to a declined quality of disease surveillance, leading to fewer cases being detected and more underreporting. Moreover, milder cases of disease may have been undetected and therefore not reported as people were less likely to visit health care facilities to seek care for mild illness during full or partial lockdowns in countries.
Poland accounts for a high proportion of cases, but Polish authorities suggest that this may be an overestimate because many of the reported cases do not test positive in the lab. Could Poland’s data be overestimated by well-intentioned doctors?
In recent years Poland has contributed to most of the rubella cases in the Region. However, almost all these cases were not laboratory confirmed cases of rubella and were reported as clinically compatible cases. This means that they were only possible cases of rubella.
Rubella vaccine in Poland was introduced in 2004 to both females and males and was given to children 13 months old with a second dose at 10 years of age. Until then it was only given to adolescent girls. In 2013, Poland experienced a nationwide outbreak of rubella mostly affecting males aged 15-19 years. Since then, there is a tendency in Poland by well-intentioned doctors to report cases with symptoms of rubella as rubella without them being laboratory confirmed. We know very well that the symptoms of rubella such as a rash and fever are similar to those produced by other viruses such as parvovirus B-19. Hence, the importance of testing suspected cases.

Many countries of the European Region have in recent years received large numbers of refugees, asylum seekers and migrants from within and from other regions of the world. How concerning is population movement on the wider goal of improving vaccine uptake and ending the spread of vaccine-preventable diseases?
In situations where countries are receiving a large number of people from other countries it is important to establish the vaccination status of those entering the country. If their vaccination status cannot be established, for example, because of lack of documentation, then refugees, asylum seekers and migrants need to be vaccinated according to the national immunisation schedule of the host country without unnecessary delay.
Such populations are generally vaccinated but some children may have missed opportunities to be fully vaccinated when they were still living in their home country for various reasons such as disrupted immunization programmes (due to COVID-19 or conflict) or difficulties in accessing vaccines, for example, due to lack of registration with a health service provider. To prevent the occurrence of vaccine-preventable diseases high vaccination coverage is needed across all populations of the Region.
Do you believe rubella elimination in the European Region will happen?
We have a very effective and long-lasting vaccines. I passionately believe elimination of this potentially devastating disease in the Region is achievable and we should do all we can to make it happen as soon as possible.




