The post-war optimism that defined the 1950s helped intensify the fight against infectious diseases like smallpox, TB and polio.
Polio cases were surging but so too was confidence that the disease could be tamed by a vaccine.
In 1952, Jonas Salk tested the first polio vaccine, proving his injected dose of inactivated poliovirus could protect against the disease. Shortly afterwards, Albert Sabin developed an oral polio vaccine using polio virus. Human trials began in 1957 and the vaccine was licensed by 1962.
The late 1950s had also seen a major flu pandemic as a new influenza virus swept across Asia. Maurice Hilleman, a biomedical researcher at the US Department of Defense took samples of the virus from US servicemen located in the region after noticing a spike in flu cases in Hong Kong.
The strain spread rapidly, partly due to the fact that most people lacked antibody protection against the novel virus – with the exception of elderly people who had survived the 1889-1890 flu pandemic.
Hilleman was instrumental in ramping up vaccine production by sending virus samples to manufacturers and demanding that they develop a vaccine in four months. The pandemic killed two million people – although medical historians say it could have been many more but for the vaccine.
Global cooperation
It was a time when bold action was needed to turn decades of new science into a landmark moment which would capture the public imagination. Vaccination needed its ‘Moon Landing Moment’.
And so it was that the Twelfth World Health Assembly in 1959 adopted the ambitious goal of eradicating smallpox.
More than 150 years had passed since Edward Jenner had used material from a cowpox lesion to inoculate and protect a local boy and methods for improving the efficacy and production capacities of smallpox vaccines had come a long way in the interim.
Eight years later, faced by a frustratingly slow pace of progress, the World Health Organisation ramped up its efforts to meet the goal it has set itself. A multi-million dollar annual investment was pledged and the keenest minds in epidemiology were brought together to apply the most up to date methods.
The Soviet Union and United States donated the bulk of the vaccines at the beginning of the eradication drive but, with poorer countries worst affected, the WHO managed to ensure that the bulk of vaccinations were prepared locally by the early 1970s.
In Europe, the last major smallpox outbreak was in 1972 in Yugoslavia (the first in almost a decade) and by 1975 the disease persisted only in the Horn of Africa. Despite difficult local conditions, complicated by war, famine and poor infrastructure, the last naturally occurring case was recorded in October 1975.
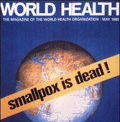
Four years later, scientists finally declared that smallpox had been eradicated. The battle was won.
A series of success stories
Smallpox remains the standout success story for vaccination. But it wasn’t the only progress seen in the second half of the 20th century. There were breakthroughs in the fight against measles, rubella, mumps and hepatitis; new vaccines for chickenpox, pneumococcal disease, diphtheria, and whooping cough as well as continued refinement of production and delivery methods.
For all of that, vaccines slowly became victims of their own success. Towards the end of the 20th century, scepticism towards vaccination – a phenomenon as old as vaccines themselves – began to flourish again.
In developed countries where diseases like smallpox and polio were eradicated or under control, and the wild scourge of measles and rubella dramatically brought to heel, the perceived danger of infection began to evaporate.
Fear and complacency
The most stark example was the MMR scare which began in the UK but soon spread to the US and beyond. A study by Andrew Wakefield published (but later retracted) by The Lancet claimed a connection between the MMR vaccine and autism.
The article sparked a public health scare and media furor, ultimately leading in some countries to a dramatic falloff in immunisation rates. A surge in measles cases followed.
Wakefield was struck off the medical register in the UK; The Lancet said elements of the research had been falsified; most of his coauthors withdrew their support; and the British Medical Journal ran a series of devastating exposés accusing him of perpetrating an “elaborate fraud”.
The damage done by the Wakefield affair and other vaccine scandals is not easily reversed. The first decade of the 21st century began with a crisis of confidence in vaccination and ended with the first influenza pandemic for four decades keeping vaccine-preventable diseases in the headlines.
Today, in light of the sometimes deadly impact of misplaced vaccine fears, there are signs of pushback. Doctors, journalists and public authorities are putting their heads above the parapet to speak up for vaccines.
History in the making
This History of Vaccines series has illustrated the game-changing impact that vaccines have had on society. Infant mortality, maternal death, life expectancy – all have been improved by vaccines.
In just a couple of centuries we have left behind an era where losing several family members to infectious diseases was routine in every corner of the globe. The challenge remains to ensure that people all over the world, rich and poor, can share in this success story.
It is also clear that vaccines for a host of deadly diseases remain out of reach for now. Embracing the optimism that prevailed in the 1950s – and pairing it with modern molecular biology and further investment in research – should give us reason to hope.
Sources:
www.historyofvaccines.org
Ian Glynn and Jenifer Glynn, The Life and Death of Smallpox
Matthew Maty, The Advantages of Early Inoculation
Michael B. A Oldstone, Viruses, Plagues, & History
Herve Bazin, L’Histoire des Vaccinations
Related:
This article is part of a series compiled by Vaccines Today to raise awareness of European Immunization Week 2011 which runs from 23-30 April